Cellular Challenges: Taking an Aim at Cancer
Immunotherapy is a powerful treatment that harnesses the body’s immune system in the fight against cancer. With optimized cell therapy, the result is an expanded population of T cells primed to recognize and eradicate malignant tumor cells that would otherwise escape immune detection.

Leukapheresis
White blood cells are separated from a patient’s blood sample.
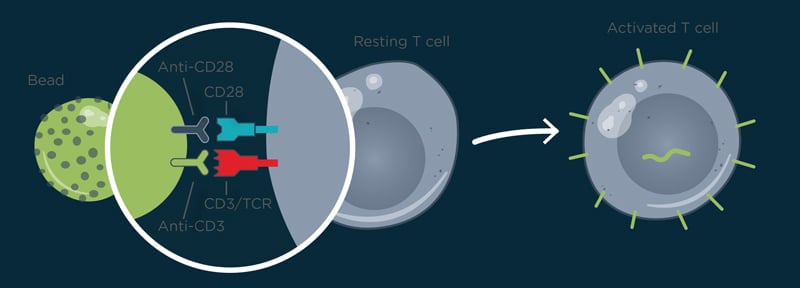
Selection and Activation
T cells are isolated from the sample via centrifugal elutriation and confirmed by Coulter analysis of cell volume. The cells are activated using magnetic beads with antibodies against CD3 and CD28. Coulter analysis is used to monitor the transition from resting T cells to activated T cells, by tracking the accompanying increase in cell volume.

Transduction
Viral vectors, such as a lentiviral or retroviral vectors, insert genes expressing cancer-targeting chimeric antigen receptors (CARs) into T cells. The CAR consists of an antigen-recognition exodomain and costimulatory signaling domains that amplify T-cell activation.

Cell Expansion
Ex vivo expansion of cells in a bioreactor. Critical culture parameters such as cell density, size, volume, and viability are monitored daily. Mean cell volume changes can be used to monitor the population size. Once the target population size is reached, the magnetic beads are washed out and the cells concentrated.

Cell Analysis
Immunophenotyping is confirmed with flow cytometry analysis of the modified cells. Sterility, safety, and potency of the cell product are tested.
Patient Infusion
The modified T cells are infused into a conditioned patient. They search and destroy cancer cells expressing the antigen targeted by the CAR.
Products for Cell Counting

Vi-CELL BLU
Use the Vi-CELL BLU for fast, small volume viability analysis
Multisizer 4e Coulter Counter
Use the Multisizer 4e for Coulter-based counting and sizing of particles independently of their interaction with light

